Understanding PCOS (Polycystic Ovarian Syndorme)
- Sheetal Badami
- Jan 7, 2023
- 3 min read
Updated: Jan 16, 2023

PCOS was first described in 1935 by Stein and Levinthal and is also referred to as Stein- Levinthal syndrome. Few of the interesting stats about PCOS are:
It affects 1 in 5 women of reproductive age in India.
It’s the most common cause of Menstrual irregularity- 3-15%.
It is responsible for 80-90 % of anovulatory infertility cases.
Causes of PCOD
The balance between various sex hormones is disrupted leading to failure of ovulation. There is increased growth of small follicles but follicles fail to mature and ovulation doesn’t happen. These immature follicles form the cysts in the ovaries. This can further lead to irregular periods and fertility issues.
The following factors may increase the risk of developing PCOS:
Family history: PCOS tends to run in families, so individuals with a family history of the condition may be at increased risk.
Obesity: Being overweight or obese can increase the risk of PCOS.
Insulin resistance: Insulin resistance is a common feature of PCOS, and individuals with insulin resistance may be at increased risk of developing the condition.
Ethnicity: PCOS is more common in certain ethnic groups, including Hispanic, Native American, and African American women.
Early onset of puberty: Girls who start puberty at an early age may be at an increased risk of developing PCOS.
Health Issues
PCOD can lead to various health issues:
Ovarian Cysts
Weight Gain
During Adolescence- Irregular menses, Facial hair growth, Acne, Hair thinning
In Reproductive age- Infertility, Early pregnancy loss, Pregnancy induced hypertension, Gestational diabetes
During Menopause- Metabolic syndrome, Endometrial carcinoma
PCOD and Metabolic Syndrome
New research shows that it is not just a disease with infertility & irregular menses but is associated with many metabolic complications:
Obesity
Obstructive sleep apnoea
Type 2 Diabetes
Abnormal Lipid Profile
Hypertension
Cardiovascular disease
This complex of Obesity, PCOD and other metabolic complications is called as Metabolic Reproductive Syndrome
Role of Insulin
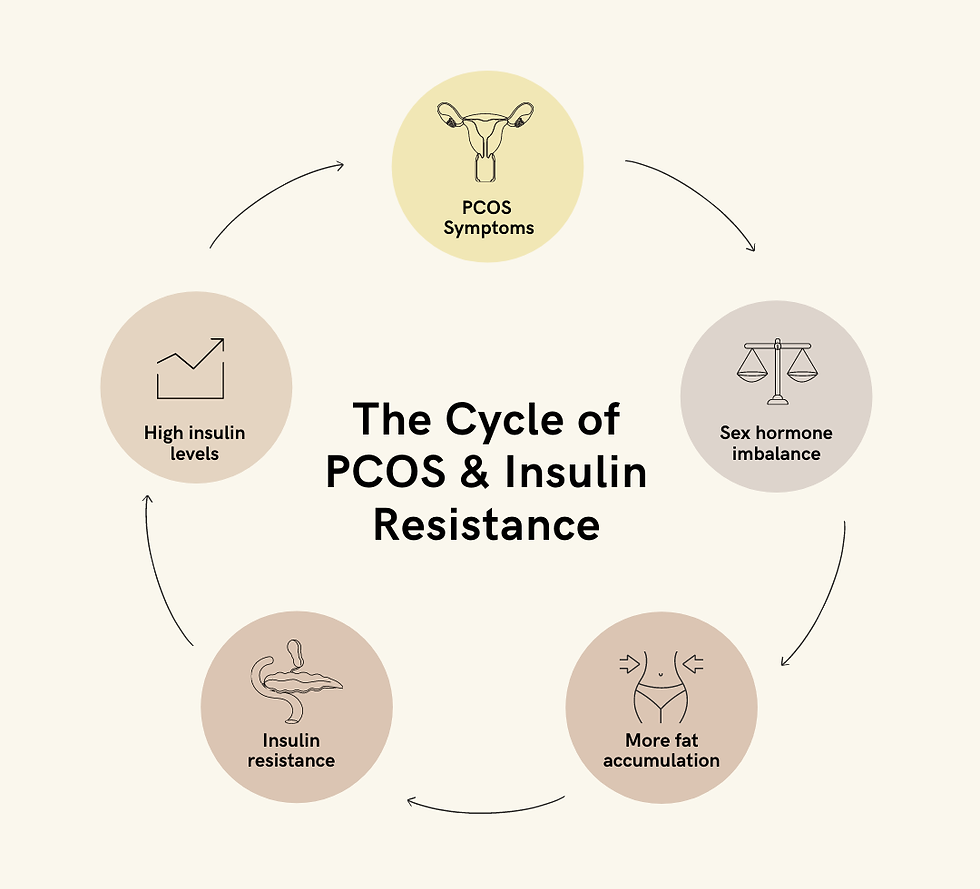
Insulin is a key hormone in the pathophysiology of PCOD. One factor that contributes to excess androgen production is insulin resistance. When your body produces too much insulin, it can lead to insulin resistance, which decreases your body’s ability to use insulin properly. When the body cannot use insulin properly, it increases glucose production, which may increase androgen production by the ovaries. Insulin resistance can also lead to weight gain and difficulty losing weight.
Statistics show that
Independent of Obesity PCOS increases abdominal fat deposition and Insulin Resistance
Obese women with PCOS have much higher Insulin levels than obese people without PCOS
Diagnosis of PCOS
Diagnosis of PCOS can be done using the following ways:
Physical examination: Physicians can look for signs of excess hair growth acne and weight gain which can be associated with PCOS
Blood tests: Blood tests can be used to measure levels of hormones such as insulin and androgens. Blood tests may also be used to check for other conditions that may cause similar symptoms, such as Thyroid dysfunction, Hyperprolactinemia, Hypothalamic causes or Cushing’s syndrome.
Ultrasound: An ultrasound exam can be used to visualize the ovaries and look for the presence of small cysts. This test is usually performed by a radiologist or a sonographer.
Any woman with PCOS should be screened for-
Obesity - BMI & WC
Insulin Resistance - HbA1C, Fasting Sugar & Fasting Insulin
Lipid profile
Re-screening every 3-5 yrs.
Management
Weight management: Weight loss normalises hormone levels. Return of ovulation is seen in 30% of cases after weight loss.
Treatment of Insulin Resistance: Treatment of insulin resistance with diet, exercise and medication if required.
Treatment for cosmetic concerns: Acne, Hair loss, and Hirsutism can be treated with various cosmetic procedures like Chemical Peel & Laser
Treatment of Infertility: Ovulation induction by Clomiphene citrate or Gonadotropins, Artificial Reproduction
Hormonal Oral Contraceptive Pills: In premenopausal women who have symptoms of androgen excess such as hirsutism and acne. May take at least 6 months for a visible effect due to the normal hair growth cycle. If there is no effect even after 6 months, anti-androgens may be added.
Content Credits

Dr Sheetal Badami
Author
コメント